- HOME
- CONSULTATIONS
- MAIN PROCEDURES
- TOPICS
- Celiac Disease
- Constipation
- Lactose Intolerance
- Cyclic Vomiting Syndrome
- H Pylori and Peptic Ulcers
- Digestive System: How it Works
- Heartburn
- Irritable Bowel Syndrome
- Polyps
- Ulcerative Colitis
- Crohn's Disease
- Gallstones
- Pancreatitis
- Hemorrhoids
- Diverticular Disease
- Abdominal Adhesions
- FODMAPs
- Non Celiac Gluten Sensitivity
- RESEARCH
- BIOGRAPHY
- LINKS
TOPICS
Ulcerative Colitis (UC)
Ulcerative colitis is a chronic, or long-lasting, disease that causes inflammation and sores, called ulcers, in the inner lining of the large intestine, which includes the colon and the rectum—the end part of the colon.
UC is one of the two main forms of chronic inflammatory disease of the gastrointestinal tract, called inflammatory bowel disease (IBD). The other form is called Crohn’s disease.
Normally, the large intestine absorbs water from stool and changes it from a liquid to a solid. In UC, the inflammation causes loss of the lining of the colon, leading to bleeding, production of pus, diarrhea, and abdominal discomfort.
-
What causes UC?
The cause of UC is unknown though theories exist. People with UC have abnormalities of the immune system, but whether these problems are a cause or a result of the disease is still unclear. The immune system protects people from infection by identifying and destroying bacteria, viruses, and other potentially harmful foreign substances. With UC, the body’s immune system is believed to react abnormally to bacteria in the digestive tract. UC sometimes runs in families and research studies have shown that certain gene abnormalities are found more often in people with UC.
UC is not caused by emotional distress, but the stress of living with UC may contribute to a worsening of symptoms. In addition, while sensitivity to certain foods or food products does not cause UC, it may trigger symptoms in some people. -
What are the Symptoms of UC?
The most common symptoms of UC are abdominal discomfort and blood or pus in diarrhea. Other symptoms include:
- anemia
- fatigue
- fever
- nausea
- weight loss
- loss of appetite
- rectal bleeding
- loss of body fluids and nutrients
- skin lesions
- growth failure in children
Most people diagnosed with UC have mild to moderate symptoms. About 10 percent have severe symptoms such as frequent fevers, bloody diarrhea, nausea, and severe abdominal cramps. UC can also cause problems such as joint pain, eye irritation, kidney stones, liver disease, and osteoporosis. Scientists do not know why these problems occur, but they think these complications may be the result of inflammation triggered by the immune system. Some of these problems go away when UC is treated. -
Who develops UC?
While UC can occur in people of any age, it usually develops between the ages of 15 and 30 and less frequently between the ages of 60 and 80. The disease affects men and women equally. People with a family member or first-degree relative with an IBD are at higher risk for developing UC, as are Caucasians and people of Jewish descent.
-
How is UC diagnosed?
Ulcerative colitis can be difficult to diagnose because its symptoms are similar to those of other intestinal disorders and to Crohn’s disease. Crohn’s disease differs from UC in that Crohn’s disease causes inflammation deeper within the intestinal wall and can occur in other parts of the digestive system, including the small intestine, mouth, esophagus, and stomach.
People with suspected UC may be referred to a gastroenterologist, also called a gastroenterological specialist, a doctor who specializes in digestive diseases. A physical exam and medical history are usually the first steps in diagnosing UC, followed by one or more tests and procedures:
- Blood tests. A blood test involves drawing blood at a health care provider’s office or commercial facility and sending the sample to a lab for analysis. The blood test can show a high white blood cell (WBC) count, which is a sign of inflammation somewhere in the body. Blood tests can also detect anemia, which could be caused by bleeding in the colon or rectum.
- Stool test. Stool tests can show WBCs, which indicate UC or another IBD. The doctor will give the person a pan and a container for catching and storing the stool. The sample is returned to the health care provider or a commercial facility and sent to a lab for analysis. The sample also allows doctors to detect bleeding or infection in the colon or rectum caused by bacteria, a virus, or parasites.
- Flexible sigmoidoscopy and colonoscopy. These tests are the most accurate methods for diagnosing UC and ruling out other possible conditions, such as Crohn’s disease, diverticular disease, or cancer. The tests are similar, but colonoscopy is used to look inside the rectum and entire colon, while flexible sigmoidoscopy is used to look inside the rectum and lower colon. For both tests, the doctor will provide written bowel prep instructions to follow at home before the test. The person may be asked to follow a clear liquid diet for 1 to 3 days before the test. A laxative may be required the night before the test. One or more enemas may be required the night before and about 2 hours before the test.
For both tests, the person lies on a table while the doctor inserts a flexible tube into the anus. A small camera on the tube sends a video image of the intestinal lining to a computer screen. The doctor can see inflammation, bleeding, or ulcers on the colon wall. The doctor may also perform a biopsy by snipping a bit of tissue from the intestinal lining. The person will not feel the biopsy. The doctor will look at the tissue with a microscope to confirm the diagnosis. These tests are performed at a hospital or outpatient center by a gastroenterologist. In most cases, a light sedative, and possibly pain medication, helps people relax. The test can show problems in the rectum or lower colon that may be causing symptoms. Cramping or bloating may occur during the first hour after the test. Driving is not permitted for 24 hours after the test to allow the sedative time to wear off. Before the appointment, a person should make plans for a ride home. Full recovery is expected by the next day. - Computerized tomography (CT) scan and barium enema x ray. A CT scan uses a combination of x rays and computer technology to create three-dimensional (3-D) images. A CT scan may include the injection of a special dye, called contrast medium. CT scans require the person to lie on a table that slides into a tunnel-shaped device where the x rays are taken. The procedure is performed in an outpatient center or hospital by an x-ray technician, and the images are interpreted by a radiologist—a doctor who specializes in medical imaging; anesthesia is not needed. A barium enema x ray involves the injection of contrast medium, called barium, into the colon to make the colon, rectum, and lower part of the small intestine more visible in x-ray images. The procedure is performed in a hospital or outpatient center by an x-ray technician, and the images are interpreted by a radiologist; anesthesia is not needed. These tests can show physical abnormalities and are sometimes used to diagnose UC.
-
How is UC treated?
Treatment for UC depends on the severity of the disease and its symptoms. Each person experiences UC differently, so treatment is adjusted for each individual.
Medication Therapy
While no medication cures UC, many can reduce symptoms. The goals of medication therapy are to induce and maintain remission—periods when the symptoms go away for months or even years—and to improve quality of life. Many people with UC require medication therapy indefinitely, unless they have their colon and rectum surgically removed.
- Aminosalicylates, medications that contain 5-aminosalicyclic acid (5-ASA), help control inflammation. Depending on which parts of the colon and rectum are affected by UC, 5-ASAs can be given orally; through a rectal suppository, a small plug of medication inserted in the rectum; or through an enema—liquid medication put into the rectum. Unless the UC symptoms are severe, people are usually first treated with aminosalicylates. These medications are also used when symptoms return after a period of remission.
- Corticosteroids, such as prednisone, methylprednisone, and hydrocortisone, also reduce inflammation. They are used for people with more severe symptoms and people who do not respond to 5-ASAs. Corticosteroids, also known as steroids, can be given orally, intravenously, or through an enema, a rectal foam, or a suppository, depending on which parts of the colon and rectum are affected by UC. Side effects include weight gain, acne, facial hair, hypertension, diabetes, mood swings, bone mass loss, and an increased risk of infection. Because of harsh side effects, steroids are not recommended for long-term use. Steroids are usually prescribed for short-term use and then stopped once inflammation is under control. The other UC medications are used for long-term symptom management.
- Immunomodulators, such as azathioprine, 6-mercaptopurine and cyclosporine suppress the immune system. These medications are prescribed for people who do not respond to 5-ASAs.
Immunomodulators are given orally, but they are slow-acting and can take 3 to 6 months to take effect. People taking these medications are monitored for complications including nausea, vomiting, fatigue, pancreatitis, hepatitis, a reduced WBC count, and an increased risk of infection. Cyclosporine is only used with severe UC, because one of its frequent side effects is toxicity, which means it can cause harmful effects to the body over time. - Infliximab is an anti-tumor necrosis factor (anti-TNF) agent prescribed to treat people who do not respond to the other UC medications or who cannot take 5-ASAs. People taking Infliximab should also take immunomodulators to avoid allergic reactions. Infliximab targets a protein called TNF that causes inflammation in the intestinal tract. The medication is given through intravenous infusion—through a vein—every 6 to 8 weeks at a hospital or outpatient center. Side effects may include toxicity and increased risk of infections, particularly tuberculosis.
Other medications may be prescribed to decrease emotional stress or to relieve pain, reduce diarrhea, or stop infection.
Hospitalization
Sometimes UC symptoms are severe enough that a person must be hospitalized. For example, a person may have severe bleeding or diarrhea that causes dehydration. In such cases, health care providers will use intravenous fluids to treat diarrhea and loss of blood, fluids, and mineral salts. People with severe symptoms may need a special diet, tube feeding, medications, or surgery.
Surgery
About 10 to 40 percent of people with UC eventually need a proctocolectomy—surgery to remove the rectum and part or all of the colon.1 Surgery is sometimes recommended if medical treatment fails or if the side effects of corticosteroids or other medications threaten a person’s health. Other times surgery is performed because of massive bleeding, severe illness, colon rupture, or cancer risk. Surgery is performed at a hospital by a surgeon; anesthesia will be used. Most people need to remain in the hospital for 1 to 2 weeks, and full recovery can take 4 to 6 weeks.
A proctocolectomy is followed by one of the following operations:
- Ileoanal pouch anastomosis, also called “pouch surgery,” makes it possible for people with UC to have normal bowel movements, because it preserves part of the anus. For this operation, the surgeon preserves the outer muscles of the rectum during the proctocolectomy. The ileum—the lower end of the small intestine—is then pulled through the remaining rectum and joined to the anus, creating a pouch. Waste is stored in the pouch and passes through the anus in the usual manner. Bowel movements may be more frequent and watery than before the procedure. Inflammation of the pouch, called pouchitis, is a possible complication and can lead to symptoms such as increased diarrhea, rectal bleeding, and loss of bowel control. Pouch surgery is the first type of surgery considered for UC because it avoids a long-term ileostomy.
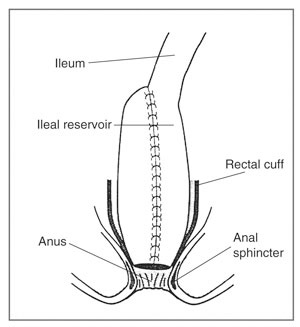 Ileoanal pouch Anastomosis
Ileoanal pouch Anastomosis
- Ileostomy is an operation that attaches the ileum to an opening made in the abdomen, called a stoma. The stoma is about the size of a quarter and is usually located in the lower right part of the abdomen near the beltline. An ostomy pouch is then attached to the stoma and worn outside the body to collect stool. The pouch needs to be emptied several times a day. An ileostomy performed for UC is usually permanent. A specially trained nurse will teach the person how to clean, care for, and change the ostomy pouch and how to protect the skin around the stoma.
The type of surgery recommended will be based on the severity of the disease and the person’s needs, expectations, and lifestyle. People faced with this decision should get as much information as possible by talking with their doctors; enterostomal therapists, nurses who work with colon surgery patients; other health care professionals; and people who have had colon surgery. Patient advocacy organizations can provide information about support groups and other resources. -
Eating, Diet, and Nutrition
Dietary changes may help reduce UC symptoms. A recommended diet will depend on the person’s symptoms, medications, and reactions to food. General dietary tips that may alleviate symptoms include:
- eating smaller meals more often
- avoiding carbonated drinks
- eating bland foods
- avoiding high-fiber foods such as corn and nuts
For people with UC who do not absorb enough nutrients, vitamin and nutritional supplements may be recommended. -
Is Colon Cancer a concern with UC?
People with UC have an increased risk of colon cancer when the entire colon is affected for a long period of time. For example, if only the lower colon and rectum are involved, the risk of cancer is no higher than that of a person without UC. But if the entire colon is involved, the risk of cancer is higher than the normal rate.4 The risk of colon cancer also rises after having UC for 8 to 10 years and continues to increase over time. Effective maintenance of remission by treatment of UC may reduce the risk of colon cancer. Surgical removal of the colon eliminates the risk of colon cancer. With UC, precancerous changes—called dysplasia—sometimes occur in the cells lining the colon. People with dysplasia are at increased risk of developing colon cancer. Doctors look for signs of dysplasia when performing a colonoscopy or flexible sigmoidoscopy and when examining tissue removed during these procedures.
According to the U.S. Preventive Services Task Force guidelines for colon cancer screening, people who have had IBD throughout the colon for at least 8 years and those who have had IBD in only the left side of the colon for 12 to 15 years should have a colonoscopy with biopsies every 1 to 2 years to check for dysplasia. Such screening has not been proven to reduce the risk of colon cancer, but it may help identify cancer early and improve prognosis. These guidelines were produced by an independent expert panel and endorsed by numerous organizations, including the American Cancer Society, the American College of Gastroenterology, the American Society of Colon and Rectal Surgeons, and the Crohn’s & Colitis Foundation of America.
Points to remember:
- Ulcerative colitis (UC) is a chronic, or long-lasting, disease that causes inflammation and sores, called ulcers, in the inner lining of the colon and rectum.
- Ulcerative colitis is one of the two main forms of chronic inflammatory disease of the gastrointestinal tract, called inflammatory bowel disease (IBD).
- The most common symptoms of UC are abdominal discomfort and bloody diarrhea.
- Flexible sigmoidoscopy and colonoscopy are the most accurate methods for diagnosing UC and ruling out other possible conditions, such as Crohn’s disease, diverticular disease, or cancer.
- Treatment for UC depends on the severity of the disease and its symptoms. Each person experiences UC differently, so treatment is adjusted for each individual. Treatment may include medication therapy, hospitalization, or surgery to remove the rectum and part or all of the colon.
- Most people with UC never develop colon cancer, but two factors that increase the risk are the duration of the disease and how much of the colon is affected.
OTHER TOPICS
Celiac Disease
Constipation
Lactose Intolerance
Cyclic Vomiting Syndrome (CVS)
H Pylori and Peptic Ulcers
Digestive System: How it Works
Heartburn
Irritable Bowel Syndrome
Polyps
Ulcerative Colitis
Crohn's Disease
Gallstones
Pancreatitis
Hemorrhoids
Diverticular Disease
Abdominal Adhesions
FODMAPs
Non Celiac Gluten Sensitivity

