- HOME
- CONSULTATIONS
- MAIN PROCEDURES
- TOPICS
- Celiac Disease
- Constipation
- Lactose Intolerance
- Cyclic Vomiting Syndrome
- H Pylori and Peptic Ulcers
- Digestive System: How it Works
- Heartburn
- Irritable Bowel Syndrome
- Polyps
- Ulcerative Colitis
- Crohn's Disease
- Gallstones
- Pancreatitis
- Hemorrhoids
- Diverticular Disease
- Abdominal Adhesions
- FODMAPs
- Non Celiac Gluten Sensitivity
- RESEARCH
- BIOGRAPHY
- LINKS
TOPICS
Crohn’s Disease
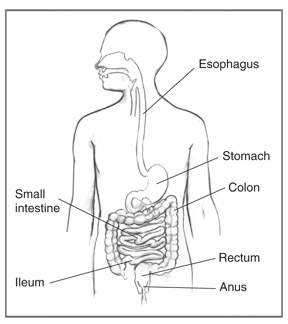
GI tract
Crohn’s disease is a disease that causes inflammation, or swelling, and irritation of any part of the digestive tract—also called the gastrointestinal (GI) tract. The part most commonly affected is the end part of the small intestine, called the ileum.
The GI tract is a series of hollow organs joined in a long, twisting tube from the mouth to the anus. The movement of muscles in the GI tract, along with the release of hormones and enzymes, allows for the digestion of food.
In Crohn’s disease, inflammation extends deep into the lining of the affected part of the GI tract. Swelling can cause pain and can make the intestine—also called the bowel—empty frequently, resulting in diarrhea. Chronic—or long-lasting—inflammation may produce scar tissue that builds up inside the intestine to create a stricture. A stricture is a narrowed passageway that can slow the movement of food through the intestine, causing pain or cramps.
Crohn’s disease is an inflammatory bowel disease (IBD), the general name for diseases that cause inflammation and irritation in the intestines. Crohn’s disease can be difficult to diagnose because its symptoms are similar to other intestinal disorders, such as ulcerative colitis and other IBDs, and irritable bowel syndrome. For example, ulcerative colitis and Crohn’s disease both cause abdominal pain and diarrhea.
Crohn’s disease may also be called ileitis or enteritis.
-
Who gets Crohn’s Disease?
Crohn’s disease affects men and women equally and seems to run in some families. People with Crohn’s disease may have a biological relative—most often a brother or sister—with some form of IBD. Crohn’s disease occurs in people of all ages, but it most commonly starts in people between the ages of 13 and 30. Men and women who smoke are more likely than nonsmokers to develop Crohn’s disease. People of Jewish heritage have an increased risk of developing Crohn’s disease.
-
What causes Crohn’s Disease?
The cause of Crohn’s disease is unknown, but researchers believe it is the result of an abnormal reaction by the body’s immune system. Normally, the immune system protects people from infection by identifying and destroying bacteria, viruses, or other potentially harmful foreign substances. Researchers believe that in Crohn’s disease the immune system attacks bacteria, foods, and other substances that are actually harmless or beneficial. During this process, white blood cells accumulate in the lining of the intestines, producing chronic inflammation, which leads to ulcers, or sores, and injury to the intestines.
Researchers have found that high levels of a protein produced by the immune system, called tumor necrosis factor (TNF), are present in people with Crohn’s disease. However, researchers do not know whether increased levels of TNF and abnormal functioning of the immune system are causes or results of Crohn’s disease. Research shows that the inflammation seen in the GI tract of people with Crohn’s disease involves several factors: the genes the person has inherited, the person’s immune system, and the environment. -
What are the symptoms of Crohn’s Disease?
The most common symptoms of Crohn’s disease are abdominal pain, often in the lower right area, and diarrhea. Rectal bleeding, weight loss, and fever may also occur. Bleeding may be serious and persistent, leading to anemia—a condition in which red blood cells are fewer or smaller than normal, which means less oxygen is carried to the body’s cells. The range and severity of symptoms varies.
-
How is Crohn’s Disease diagnosed?
A doctor will perform a thorough physical exam and schedule a series of tests to diagnose Crohn’s disease.
- Blood tests can be used to look for anemia caused by bleeding. Blood tests may also uncover a high white blood cell count, which is a sign of inflammation or infection somewhere in the body. Blood is drawn at a health care provider’s office or commercial facility and sent to a lab for analysis.
- Stool tests are commonly done to rule out other causes of GI diseases, such as infection. Stool tests can also show if there is bleeding in the intestines. The doctor will give the person a container for catching and storing the stool. The sample is returned to the doctor or a commercial facility and sent to a lab for analysis.
The tests below are usually performed at a hospital or outpatient center by a gastroenterologist, a doctor who specializes in digestive diseases, or a radiologist, a doctor who specializes in medical imaging. - Flexible sigmoidoscopy and colonoscopy. These tests are used to help diagnose Crohn’s disease and determine how much of the GI tract is affected. Colonoscopy is the most commonly used test to specifically diagnose Crohn’s disease. Colonoscopy is used to view the ileum, rectum, and the entire colon, while flexible sigmoidoscopy is used to view just the lower colon and rectum. For both tests, a health care provider will provide written bowel prep instructions to follow at home before the test. The person may be asked to follow a clear liquid diet for 1 to 3 days before the test. A laxative may be required the night before the test. One or more enemas may be required the night before and about 2 hours before the test.
For either test, the person will lie on a table while the doctor inserts a flexible tube into the anus. A small camera on the tube sends a video image of the intestinal lining to a computer screen. The doctor can see inflammation, bleeding, or ulcers on the colon wall. The doctor may also perform a biopsy by snipping a bit of tissue from the intestinal lining. The person will not feel the biopsy. The doctor will look at the tissue with a microscope to confirm the diagnosis. For a colonoscopy, a light sedative—and possibly pain medication—helps people relax.
Cramping or bloating may occur during the first hour after the test. Driving is not permitted for 24 hours after a colonoscopy to allow the sedative time to wear off. Before the appointment, people should make plans for a ride home. Full recovery is expected by the next day.
The tests below are performed at a hospital or outpatient center by an x-ray technician, and the images are interpreted by a radiologist. - Computerized tomography (CT) scan. CT scans use a combination of x rays and computer technology to create three-dimensional (3-D) images. For a CT scan, the person may be given a solution to drink and an injection of a special dye, called contrast medium. CT scans require the person to lie on a table that slides into a tunnel-shaped device where the x rays are taken. CT scans can be used to help diagnose Crohn’s disease. Children may be given a sedative to help them fall asleep for the test.
- Upper GI series. An upper GI series may be done to look at the small intestine. No eating or drinking is allowed for 8 hours before the procedure, if possible. During the procedure, the person will stand or sit in front of an x-ray machine and drink barium, a chalky liquid. Children may be given a sedative to help them fall asleep for the test. Children who are sedated will lie on a table for the test. Barium coats the small intestine, making signs of Crohn’s disease show up more clearly on x rays. A person may experience bloating and nausea for a short time after the test. For several days afterward, barium liquid in the GI tract causes stools to be white or light colored. A health care provider will provide specific instructions about eating and drinking after the test.
- Lower GI series. A lower GI series may be done to look at the large intestine. A health care provider may provide written bowel prep instructions to follow at home before the test. The person may be asked to follow a clear liquid diet for 1 to 3 days before the procedure. A laxative or enema may be used before the test. A laxative is medication that loosens stool and increases bowel movements. An enema involves flushing water, laxative, or sometimes a mild soap solution into the anus using a special squirt bottle. Children may be given a sedative to help them fall asleep for the test. For the test, the person will lie on a table while the doctor inserts a flexible tube into the person’s anus. The large intestine is filled with barium, making signs of Crohn’s disease show up more clearly on x rays.
For several days afterward, traces of barium liquid in the large intestine cause stools to be white or light colored. Enemas and repeated bowel movements may cause anal soreness. A health care provider will provide specific instructions about eating and drinking after the test.
-
What are the complications of Crohn’s Disease?
The most common complication of Crohn’s disease is an intestinal blockage caused by thickening of the intestinal wall because of swelling and scar tissue. Crohn’s disease may also cause ulcers that tunnel through the affected area into surrounding tissues. The tunnels, called fistulas, are a common complication—especially in the areas around the anus and rectum—and often become infected. Most fistulas can be treated with medication, but some may require surgery. In addition to fistulas, small tears called fissures may develop in the lining of the mucus membrane of the anus. The health care provider may prescribe a topical cream and may suggest soaking the affected area in warm water.
Some Crohn’s disease complications occur because the diseased area of intestine does not absorb nutrients effectively, resulting in deficiencies of proteins, calories, and vitamins.
People with Crohn’s disease often have anemia, which can be caused by the disease itself or by iron deficiency. Anemia may make a person feel tired. Children with Crohn’s disease may fail to grow normally and may have low height for their age.
People with Crohn’s disease, particularly if they have been treated with steroid medications, may have weakness of their bones called osteoporosis or osteomalacia.
Some people with Crohn’s disease may have restless legs syndrome—extreme leg discomfort a person feels while sitting or lying down. Some of these problems clear up during treatment for Crohn’s disease, but some must be treated separately.
Other complications include arthritis, skin problems, inflammation in the eyes or mouth, kidney stones, gallstones, or diseases related to liver function. -
What is the treatment for Crohn’s Disease?
Treatment may include medications, surgery, nutrition supplementation, or a combination of these options. The goals of treatment are to control inflammation, correct nutritional deficiencies, and relieve symptoms such as abdominal pain, diarrhea, and rectal bleeding. Treatment for Crohn’s disease depends on its location, severity, and complications.
Treatment can help control Crohn’s disease and make recurrences less frequent, but no cure exists. Someone with Crohn’s disease may need long-lasting medical care and regular doctor visits to monitor the condition. Some people have long periods—sometimes years—of remission when they are free of symptoms, and predicting when a remission may occur or when symptoms will return is not possible. This changing pattern of the disease makes it difficult to be certain a treatment has helped.
Despite possible hospitalizations and the need to take medication for long periods of time, most people with Crohn’s disease have full lives—balancing families, careers, and activities.
Medications
Anti-inflammation medications. Most people are first treated with medications containing 5-aminosalicylic acid (5-ASA) agents, such as Asacol, Dipentum, or Pentasa. Possible side effects of include nausea, vomiting, heartburn, diarrhea, and headache.
Cortisone or steroids. These medications, also called corticosteroids, are effective at reducing inflammation. Prednisone and budesonide are generic names of two corticosteroids. During the earliest stages of Crohn’s disease, when symptoms are at their worst, corticosteroids are usually prescribed in a large dose. The dosage is then gradually lowered once symptoms are controlled. Corticosteroids can cause serious side effects, including greater susceptibility to infection and osteoporosis, or weakening of the bones. See the “Nutrition Supplementation” section for more information about preventing and treating osteoporosis.
Immune system suppressors. Medications that suppress the immune system—called immunosuppressive medications—are also used to treat Crohn’s disease. The most commonly prescribed medications are 6-mercaptopurine and azathioprine. Immunosuppressive medications work by blocking the immune reaction that contributes to inflammation. These medications may cause side effects such as nausea, vomiting, and diarrhea and may lower a person’s resistance to infection. Some people are treated with a combination of corticosteroids and immunosuppressive medications. Some studies suggest that immunosuppressive medications may enhance the effectiveness of corticosteroids.
Biological therapies. Biological therapies are medications given by an injection in the vein, infliximab, or an injection in the skin, adalimumab. Biological therapies bind to TNF substances to block the body’s inflammation response. The U.S. Food and Drug Administration approved these medications for the treatment of moderate to severe Crohn’s disease that does not respond to standard therapies—mesalamine substances, corticosteroids, immunosuppressive medications—and for the treatment of open, draining fistulas. Some studies suggest that biological therapies may enhance the effectiveness of immunosuppressive medications.
Antibiotics. Antibiotics are used to treat bacterial overgrowth in the small intestine caused by stricture, fistulas, or surgery. For this common problem, the doctor may prescribe one or more of the following antibiotics: ampicillin, sulfonamide, cephalosporin, tetracycline, or metronidazole.
Anti-diarrheal medications and fluid replacements. Diarrhea and abdominal cramps are often relieved when the inflammation subsides, but additional medication may be needed. Anti-diarrheal medications include diphenoxylate, loperamide, and codeine. People with diarrhea should drink plenty of fluids to prevent dehydration. If diarrhea does not improve, the person should see the doctor promptly for possible treatment with intravenous fluids.
Surgery
About two-thirds of people with Crohn’s disease will require surgery at some point in their lives.3 Surgery becomes necessary to relieve symptoms that do not respond to medical therapy or to correct complications such as intestinal blockage, perforation, bleeding, or abscess—a painful, swollen, pus-filled area caused by infection. Surgery to remove part of the intestine can help people with Crohn’s disease, but it does not eliminate the disease. People with Crohn’s disease commonly need more than one operation because inflammation tends to return to the area next to where the diseased intestine was removed.
- Proctocolectomy. Some people who have Crohn’s disease must have a proctocolectomy, a procedure that is performed by a specialized surgeon. Proctocolectomy is surgery to remove the rectum and part of the colon or the entire colon. People will receive sedation and general anesthesia during surgery. Most people need to remain in the hospital for 1 to 2 weeks, and full recovery can take 4 to 6 weeks.
- Ileostomy. During proctocolectomy, the surgeon also performs an ileostomy—an operation that attaches the ileum to an opening made in the abdomen called a stoma. The stoma is about the size of a quarter and is usually located in the lower right part of the abdomen near the beltline. An ostomy pouch is then attached to the stoma and worn outside the body to collect stool. The pouch needs to be emptied several times a day. A specially trained nurse will teach the person how to clean, care for, and change the ostomy pouch and how to protect the skin around the stoma. The majority of people with an ostomy pouch are able to live normal, active lives.
- Intestinal resection surgery. Sometimes only the diseased section of intestine is removed and an ileostomy is not needed. Instead, the intestine is cut above and below the diseased area and the ends of the healthy sections are connected in an operation called an intestinal resection. People will receive sedation and general anesthesia during surgery. Most people need to remain in the hospital for several days, and full recovery can take 3 to 4 weeks.
Because Crohn’s disease often recurs after surgery, people considering surgery should carefully weigh its benefits and risks compared with other treatments. People faced with this decision should get information from health care providers who routinely work with GI patients, including those who have had intestinal surgery. Patient advocacy organizations can suggest support groups and other information resources.
Nutrition Supplementation
The health care provider may recommend nutritional supplements, especially for children whose growth has been slowed. Special high-calorie liquid formulas are sometimes used. A small number of people may receive nutrition intravenously for a brief time through a small tube inserted into an arm vein. This procedure can help people who need extra nutrition temporarily, such as those whose intestines need to rest, or those whose intestines cannot absorb enough nutrition from food.
The doctor may prescribe calcium, vitamin D, and other medications to prevent or treat osteoporosis for patients taking corticosteroids. People should take vitamin supplements only after talking with their doctor.
Eating, Diet, and Nutrition
No special diet has been proven effective for preventing or treating Crohn’s disease, but it is important that people who have Crohn’s disease follow a nutritious diet and avoid any foods that seem to worsen symptoms. People with Crohn’s disease often experience a decrease in appetite, which can affect their ability to receive the daily nutrition needed for good health and healing. In addition, Crohn’s disease is associated with diarrhea and poor absorption of necessary nutrients. Foods do not cause Crohn’s disease, but foods such as bulky grains, hot spices, alcohol, and milk products may increase diarrhea and cramping. The health care provider may refer a person with Crohn’s disease to a dietitian for guidance about meal planning. -
Can smoking make Crohn’s Disease worse?
Studies have shown that people with Crohn’s disease who smoke may have more severe symptoms and increased complications of the disease, along with a need for higher doses of steroids and other medications. People with Crohn’s disease who smoke are also more likely to need surgery. Quitting smoking can greatly improve the course of Crohn’s disease and help reduce the risk of complications and flare ups. A health care provider can assist people in finding a smoking cessation specialist.
-
Can stress make Crohn’s Disease worse?
No evidence shows that stress causes Crohn’s disease. However, people with Crohn’s disease sometimes feel increased stress in their lives because they live with a chronic illness. Some people with Crohn’s disease report having a flare up when experiencing a stressful event or situation. For people who find there is a connection between stress level and a worsening of symptoms, using relaxation techniques—such as slow breathing—and taking special care to eat well and get enough sleep may help them feel better. The health care provider may suggest a counselor or support group to help decrease stress for people with Crohn’s disease.
-
Is pregnancy safe for women with Crohn’s Disease?
Women with Crohn’s disease can become pregnant and have a baby. Even so, women with Crohn’s disease should talk with their health care provider before getting pregnant. Most children born to women with Crohn’s disease are not affected by the condition.
Points to remember:
- Crohn’s disease is a disease that causes inflammation, or swelling, and irritation of any part of the digestive tract—also called the gastrointestinal (GI) tract.
- Crohn’s disease affects men and women equally and seems to run in some families.
- The cause of Crohn’s disease is unknown, but researchers believe it is the result of an abnormal reaction by the immune system.
- The most common symptoms of Crohn’s disease are abdominal pain and diarrhea.
- A doctor can diagnose Crohn’s disease by performing a physical exam, blood and stool tests, and imaging tests such as a CT scan, upper GI series, lower GI series, flexible sigmoidoscopy, and colonoscopy.
- The most common complication of Crohn’s disease is an intestinal blockage caused by thickening of the intestinal wall because of swelling and scar tissue.
- Doctors treat Crohn’s disease with medications, surgery, nutrition supplementation, or a combination of these options.
- No special diet has been proven effective for preventing or treating Crohn’s disease, but it is important that people who have Crohn’s disease follow a nutritious diet and avoid any foods that seem to worsen symptoms.
- Some people with Crohn’s disease report having a flare up when experiencing a stressful event or situation. The health care provider may suggest a counselor or support group to help decrease stress for people with Crohn’s disease.
- Women with Crohn’s disease can become pregnant and have a baby. Even so, women with Crohn’s disease should talk with their health care provider before getting pregnant
OTHER TOPICS
Celiac Disease
Constipation
Lactose Intolerance
Cyclic Vomiting Syndrome (CVS)
H Pylori and Peptic Ulcers
Digestive System: How it Works
Heartburn
Irritable Bowel Syndrome
Polyps
Ulcerative Colitis
Crohn's Disease
Gallstones
Pancreatitis
Hemorrhoids
Diverticular Disease
Abdominal Adhesions
FODMAPs
Non Celiac Gluten Sensitivity

